ED Nurses' Jobs Change Daily with COVID-19
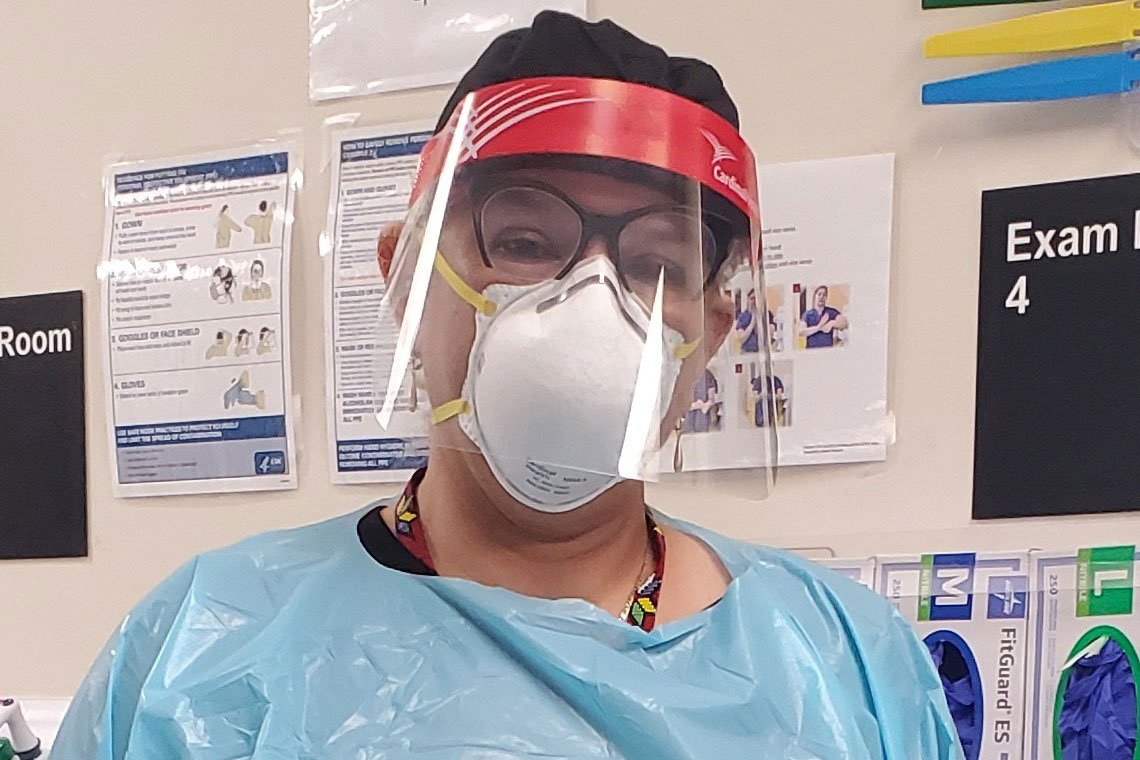
(April 8, 2020) HOUSTON - Elda Ramirez, PhD, ENP-C, directed student nurses at the George R. Brown Convention Center who cared for people displaced by Hurricanes Katrina and Harvey, but in her 30 years as an emergency department (ED) nurse, she has never seen anything like COVID-19.
“In Houston, we are used to disasters, but this one is very different,” Ramirez said.
Students from Cizik School of Nursing at The University of Texas Health Science Center at Houston (UTHealth) can’t step up to assist in treating patients the way they would in response to a hurricane. Clinical assignments have been canceled, and classes have moved online to protect students and stem the spread of the virus. However, approximately 60 Nurse Practitioner (NP) graduate students are already licensed, experienced, and working on the front lines of the pandemic.
Ramirez herself practices in three different Houston-area emergency departments, and she says every shift is different. “Things change every day based on what we are learning about the virus, and each facility uses different methods to communicate,” said Ramirez. “We must be very flexible.”
Gus Calvillo, RN, shifted from the ED environment to The University of Texas Medical Branch at Galveston’s urgent care clinic in Texas City last summer while working toward his Family Nurse Practitioner (FNP) degree. In the early days of the outbreak, the clinic tested a handful of patients each shift. That quickly shot up to 80-100.
“It feels like I’ve been dealing this for months now, but it’s really only been about 2 ½ weeks,” Calvillo said recently.
Amanda Sanger, NP, had also moved away from the ED to better balance work and school, switching to a post-anesthesia care unit instead. She is one of Ramirez’s students in the Emergency NP (ENP) post-master’s program. With clinical assignments and elective surgeries canceled on the same day, Sanger shifted back to working in Memorial Hermann Health System’s floating pool for ED staff.
Anxiety is obviously high among the patients. With allergy season in full swing, every cough is a cause for worry, Calvillo noted.
For Sanger, who worked a recent shift at a screening checkpoint outside the ED at Memorial Hermann-Texas Medical Center, one of the most emotional moments was watching a positive-tested husband and his wife “air hug,” knowing they could not be together during his hospitalization.
Nurses, too, must overcome understandable fear to treat patients at this time. Even before the COVID-19 outbreak, Calvillo had begun taking extra precautions at work to prevent bringing home any germs to his 3-month-old son and first child, Theodore, and wife, Rebecca. His co-workers now follow his lead in donning PPE.
“I’m wearing mine all of the time because we just don’t know who might have it,” said Sanger. She and her husband Damon, chief pilot for Memorial Hermann Life Flight, are also being extra careful to protect their daughters, 5-year-old Victoria and 3 ½-year-old Charlotte.
“I come home, I take everything off at the door, I drop it in the wash, I take a shower,” Calvillo said. Refraining from holding his son is the hardest part of the pandemic for Calvillo.
Meanwhile, Ramirez strives to keep students like Sanger and Calvillo up to date with their coursework through what she calls “rolling information sessions.” She presents the same information in three or four different sessions and records them so that her working students have multiple opportunities to access the material covered.
“I want to communicate with my students directly and not just by email,” she said. “You need to have contact with people.” She also tries to break up her Webex sessions so as not to overwhelm her students with hours of sitting in front of a computer.
In addition to using technology to facilitate course work, Ramirez uses video chats to keep in touch with members of the American Academy of Emergency Nurse Practitioners (AAENP), of which she is a founding member. Directors and state representatives of the organization participate in virtual meetings every other day.
Sometimes the AAENP members help one another locate resources or overcome administrative hurdles. Other times they serve as a support group, sharing common frustrations like having to turn away people who don’t meet the criteria for COVID-19 testing.
For some medical professionals, the mental health concerns posed by the pandemic stem not from the stresses and fears associated with providing care to patients, but from being unable to help if they are quarantined because of exposure, Ramirez said.
“We are doers. When you enclose someone who is a doer in a place where they can’t do, that affects us mentally,” she explained. To help combat feelings of isolation and helplessness, her AAENP group planned a Zoom social hour over the weekend. “We are trying to do what we can for the people who are on the front lines.”
Pandemic checklist for ED nurses:
Ramirez offers these suggestions for nurses on the front lines of the COVID-19 response.
- Read what is pertinent to your work, but avoid information overload.
- Review the latest updates from your hospital before each shift.
- Call ahead to check on any revisions to procedures or guidelines.
- Arrive early to make sure you have the equipment and supplies you need.
- Take your temperature regularly.
- Take care of yourself – don’t neglect hydration, nutrition, and the need for rest.
- If you don’t feel well, stay home.
- Change clothes, clean your cell phone and car surfaces, and take other precautions after your shift to keep your home environment safe.
Sherri Deatherage Green