NIH grant funds large-scale pain relief study Kawi expands research of nonpharmacological intervention in rural areas
A new $5.98 million federal grant will enable large-scale testing of a self-managed auricular point acupressure intervention for nonpharmaceutical pain management in rural areas, led by Jennifer Kawi, PhD, MSN, FNP-BC, CNE, FAAN, the Lee and Joseph Jamail Distinguished Professor at Cizik School of Nursing at UTHealth Houston.
The four-year study, “Personalized Auricular Point Acupressure for Chronic Pain Self-Management in Rural Populations (UH3AT012728),” is funded by an award from the National Center for Complementary and Integrative Health and the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH). The award is part of the NIH’s Helping to End Addiction Long-term® (HEAL) Initiative.
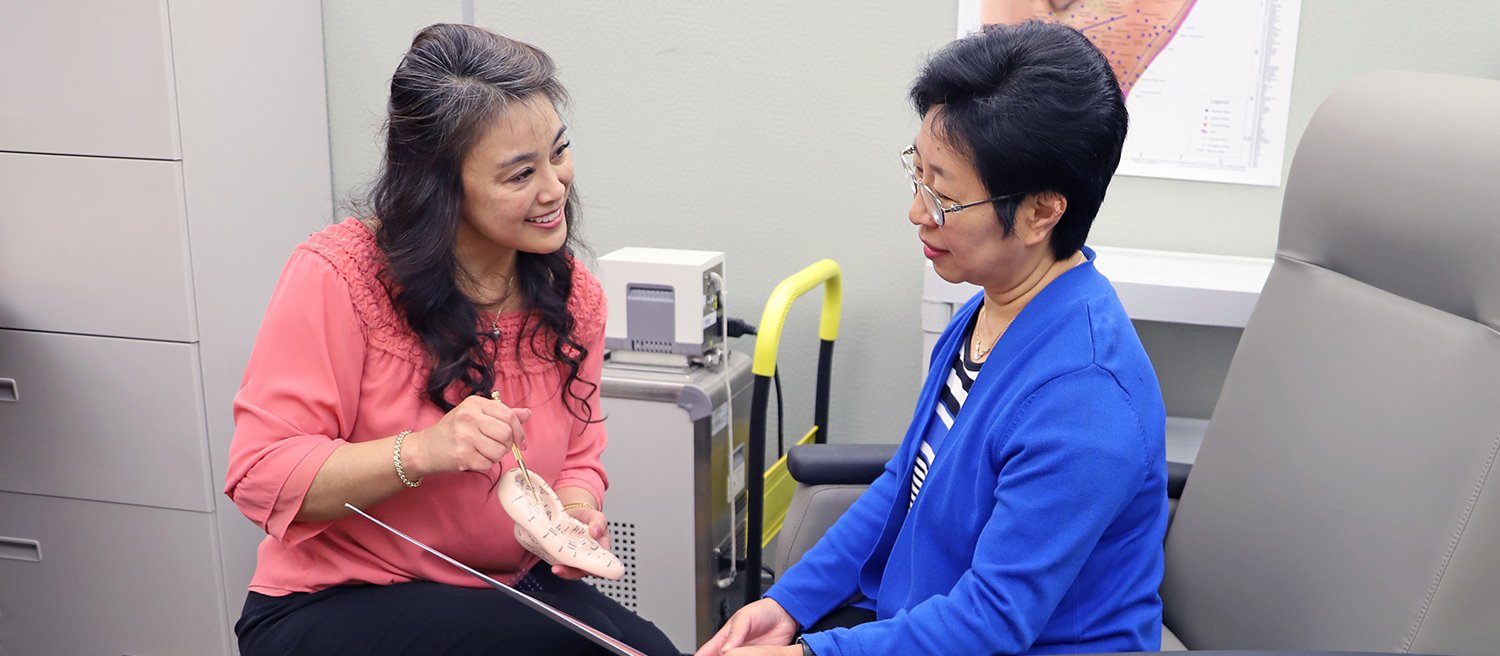
Auricular point acupressure involves stimulating specific points on the ear that correspond to body parts in pain. Pressure is applied to small seeds secured to standardized areas on patients’ ears based on their pain location. Evidence is supported in previous studies with sustained effect on pain relief and physical function.
“The literature shows that the clinical effects of auricular point acupressure are likely through modulation of brain networks involved in chronic pain and through immunological pathways,” Kawi said. “We believe a self-managed approach to auricular point acupressure can lead to transformational change in pain management, particularly by increasing access to pain care among rural populations.”
The project began in 2024 when Kawi was awarded a cooperative “U-series” grant to lay the groundwork for a large-scale, multisite, pragmatic, randomized controlled trial among rural populations with chronic musculoskeletal pain using a hybrid implementation-effectiveness approach. The initial study, UG3AT012728, is now complete, and Kawi’s interdisciplinary team is moving to the next phase, which will involve recruiting nearly 700 patients in Texas and South Carolina who are living with chronic musculoskeletal pain.
Kawi stressed the pragmatic aspect of the study. “We aren’t just focusing on whether the intervention works but on other important questions, such as accessibility, sustainability, cost-effectiveness, and which group of patients best respond to auricular point acupressure for pain relief to enhance precision medicine,” she said.
Kawi’s team uses English and Spanish versions of a smartphone app to support patients in self-administering and self-monitoring auricular point acupressure. Participants will be randomized into three groups – auricular point acupressure with in-person training, auricular point acupressure with remote training, and a control group receiving pain education and self-management skills.
Since frequent office visits and costly treatments are not practical for many rural patients, community health workers in rural communities and other intervention coaches were trained by Kawi and her team to be able to teach patients how to self-administer auricular point acupressure anytime they need it for pain relief.
“Community health workers will be integral to the study’s success,” Kawi noted.
The team has established a community advisory board and several clinical and community partnerships in both states.
“For the past year, we have engaged with various rural stakeholders such as clinics, providers, community health workers, health care administrators and staff, patients, and policymakers to learn from them and adapt our intervention to the needs of rural communities,” Kawi said. “The key impact for this large trial is to teach our community health workers and other trained rural partners to do the intervention, so that when the study is completed, the pain-relief alternative can be sustained in the community.”
Serving as co-principal investigators on this team are Hulin Wu, PhD, the Betty Wheless Trotter Professor and Chair of the Department of Biostatistics and Data Science at the School of Public Health at UTHealth Houston; and Jane Bolin, PhD, JD, RN, senior research professor with the University of North Texas Health Science Center (UNTHSC) College of Nursing. Wu will use machine learning to analyze electronic health records, claims databases, and other sources to identify predictive factors and determine which populations may benefit most from the intervention. Dr. Bolin will lead patient recruitment efforts in rural areas of Texas.
Serving as co-investigators and site leads for the project are Peiyin Hung, PhD, MSPH, associate professor at the Arnold School of Public Health at University of South Carolina-Columbia; Tonychris Nnaka, PhD, MPH, RN, CPH, associate dean for research at the UNTHSC College of Nursing in Fort Worth; and Lorraine S. Evangelista, PhD, RN, CNS, FAAN, associate professor at the Louise Herrington School of Nursing at Baylor University.